Articles
Why Your Intermittent Fasting Might Be Masking Your IBS Instead of Healing It
If you have IBS and started intermittent fasting, you probably noticed something amazing. Your stomach stopped hurting. The bloating went away. You finally felt normal again.
But here’s a question most people don’t ask: Are you actually getting better, or are you just giving your gut a break?
This is one of the most important things to understand if you’re using fasting to manage digestive problems. And the answer might surprise you.
The Relief Trap
Let me explain this with a simple example.
Imagine you sprained your ankle. It hurts when you walk, so you decide to stay off it. After a few days of rest, the pain goes away. You feel great! But here’s the thing: your ankle didn’t heal just because you stopped walking on it. The sprain is still there. The moment you start walking normally again, the pain comes right back.
This is exactly what happens with intermittent fasting and IBS.
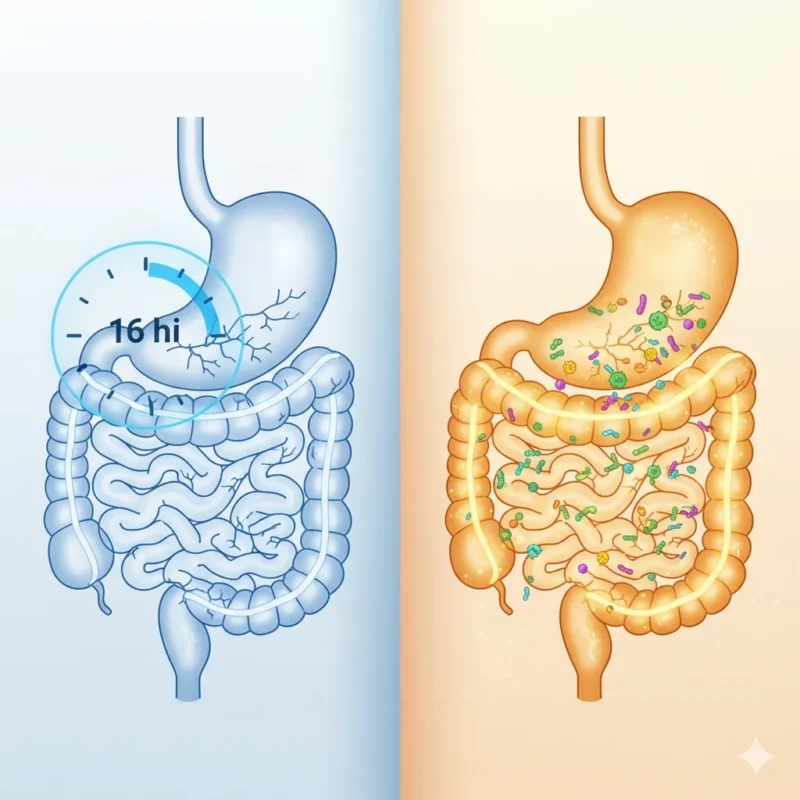
When you fast for 16, 18, or 20 hours, you’re not putting food in your system. Your gut gets a break from digesting. There’s nothing to irritate your intestines. So naturally, you feel better.
But the underlying problem, the reason your gut was sensitive in the first place, is still there. You’re just not triggering it.
What IBS Really Means
IBS stands for Irritable Bowel Syndrome. Doctors use this term when your digestive system is upset but they can’t find an obvious disease like Crohn’s or colitis.
The symptoms include stomach pain, bloating, gas, diarrhea, constipation, or switching between both. It’s uncomfortable and can really affect your quality of life.
But here’s what many people don’t realize: IBS is a symptom, not a root cause. Something is making your bowel irritable. Your gut is reacting to something.
Common triggers include bad bacteria overgrowth, yeast infections in the gut, food sensitivities, stress hormones, a damaged gut lining, or toxins that have built up in your intestines.
When you fast, you’re avoiding the triggers. But you’re not fixing what made your gut sensitive in the first place.
Why Fasting Feels So Good
During a fast, several things happen that make IBS symptoms disappear.
First, your digestive system gets a rest. When there’s no food coming in, your intestines don’t have to work. They can relax. If your gut lining is inflamed or damaged, this break feels really good.
Second, you’re not eating any trigger foods. Many people with IBS react to certain foods like dairy, gluten, high FODMAP foods, or processed ingredients. When you’re fasting, none of these foods can bother you.
Third, fasting reduces inflammation in the short term. Your immune system calms down when it’s not responding to food particles.
Fourth, your gut gets time to do some cleaning. Your intestines have a natural cleaning wave called the migrating motor complex that works best when you’re not eating.
All of this sounds great, right? And it is! Fasting does help. But there’s a big difference between feeling better and actually healing.
The Problem With Long Term Fasting For IBS
Many people get such good results from intermittent fasting that they start pushing their fasting windows longer and longer. If 16 hours feels good, maybe 20 hours is even better?
This is where things can go wrong.
First, let’s talk about your metabolism. Your body is smart. When you regularly fast for long periods, it adapts. It learns to run on less food. This sounds efficient, but it can actually slow down your metabolic rate over time. You might start feeling tired, cold, or notice your weight loss stops even though you’re eating less.
Second, there’s the muscle issue. Your body needs protein regularly to maintain muscle mass. When you compress all your eating into a short window, it’s hard to get enough protein. Even if you eat a lot in that window, your body can only use so much protein at once. The rest doesn’t get stored as muscle. Over time, you can lose muscle mass, which is bad for your metabolism and overall health.
Third, and this is really important for IBS, extended fasting can actually hurt your gut bacteria. Your microbiome, the trillions of helpful bacteria in your intestines, needs regular feeding. These bacteria eat fiber from your food. When you fast for very long periods regularly, you can reduce the diversity of your gut bacteria. For someone with IBS, having healthy, diverse gut bacteria is essential for healing.
Fourth, hormones get affected. Fasting affects cortisol (your stress hormone), thyroid hormones (which control metabolism), and sex hormones. For some people, especially women, long term fasting can disrupt menstrual cycles, reduce energy, cause hair loss, or create other hormone imbalances.
What Your Gut Actually Needs To Heal
So if fasting is just masking the problem, what’s the solution?
Real healing happens when you address why your gut became irritable in the first place. Think of it like this: if your house has a leak and you keep mopping up the water, your floor stays dry. But you haven’t fixed the leak. Eventually, the problem gets worse.
Here’s what actually helps heal IBS for good:
Remove the irritants. This means identifying what’s causing inflammation in your gut. It could be bad bacteria, yeast overgrowth, parasites, or accumulated toxins in your intestinal lining. Many people with IBS have something called SIBO, which stands for Small Intestinal Bacterial Overgrowth. This is when bacteria that should live in your large intestine end up in your small intestine where they don’t belong.
Repair the gut lining. Your intestinal wall has a protective barrier. When this barrier gets damaged, you get what’s called leaky gut. Food particles and toxins can pass through the gut wall into your bloodstream, causing inflammation and immune reactions. Healing this barrier is essential.
Restore good bacteria. Your gut needs the right balance of bacteria to digest food properly, make vitamins, and keep bad bacteria under control. This means eating foods that feed good bacteria and possibly taking quality probiotics.
Replace digestive support. Some people with IBS don’t make enough stomach acid or digestive enzymes. This means food doesn’t break down properly, which feeds bad bacteria and causes symptoms. Adding digestive support can help a lot.
Rebalance your lifestyle. Stress, poor sleep, and lack of movement all affect your gut. Your brain and gut are connected through something called the gut brain axis. When you’re stressed, your digestion suffers.
A Better Approach: Combining Fasting With Healing
The good news is you don’t have to choose between fasting and healing. You can do both.
The key is using intermittent fasting as a tool while also addressing the root causes of your IBS.
Here’s what this looks like in practice:
Keep your fasting windows moderate. Stick to 14 to 16 hours most days instead of pushing to 20 or more. This gives you the benefits of fasting without the downsides of extended fasting.
Use your eating window strategically. Focus on foods that heal and nourish your gut. This means lots of cooked vegetables, quality proteins, healthy fats, and gut healing foods like bone broth, fermented vegetables, and easy to digest starches.
Consider a cleansing protocol. Many natural health practitioners recommend doing a gut cleanse to remove built up toxins, bad bacteria, and parasites. This is something I personally explored after realizing my fasting was just managing symptoms. A structured 30 day approach helped me actually clear out what was causing my gut irritation in the first place. The combination of targeted cleansing with my moderate fasting schedule made a huge difference. For the first time, I could eat normally without immediately feeling bloated or uncomfortable. If you’re curious about what a comprehensive cleanse looks like, programs like the Full Body Cleanse are designed specifically to work through the digestive system systematically while supporting your body’s natural detox pathways.
Support your gut lining. Add supplements or foods that specifically heal the intestinal barrier. Things like L glutamine, zinc, aloe vera, and collagen can help repair damage.
Feed your good bacteria. Even during eating windows, make sure you’re eating enough fiber rich foods to keep your microbiome healthy. Your gut bacteria are your partners in healing.
Listen to your body. Some days you might need more food or shorter fasts. Other days you might naturally want to fast longer. Flexibility is important.
Signs You’re Masking Instead of Healing
How do you know if your fasting is just covering up the problem? Here are some warning signs:
Your symptoms come back immediately when you eat normally. If breaking your fast always causes bloating, pain, or digestive upset, your gut hasn’t healed. You’re just avoiding the triggers.
You can only eat certain foods without symptoms. If your list of safe foods keeps getting smaller, that’s a red flag. Healing should expand your food tolerance, not shrink it.
You feel like you have to fast to feel okay. If missing a fasting day makes you anxious or causes immediate symptoms, you’re dependent on fasting for symptom control rather than using it as a healing tool.
Your energy is decreasing over time. True healing increases energy. If you’re getting more tired, having trouble concentrating, or feeling weaker, something isn’t working.
You’re losing hair, your nails are brittle, or your skin looks dull. These are signs of nutritional deficiencies, which can happen when fasting windows are too long or when gut absorption is still impaired.
Your digestion is getting more sensitive, not less. Healing should make your gut more resilient over time. If you’re reacting to more and more foods, the underlying problem isn’t being addressed.
The Bottom Line
Intermittent fasting can be an amazing tool for managing IBS symptoms. Many people get real relief from it. But relief isn’t the same as healing.
If you want to truly heal your gut, you need to do more than just avoid triggering it. You need to address why it became irritable in the first place.
Think of fasting as one tool in your toolbox, not the only tool. Combine it with gut healing strategies that remove irritants, repair damage, restore healthy bacteria, and support your digestive function.
The goal isn’t to fast forever to avoid symptoms. The goal is to heal your gut so you can eat normally, feel great, and not have to think about your digestion all the time.
When you approach it this way, fasting becomes part of a complete healing strategy instead of just a way to manage symptoms. And that’s when real, lasting healing happens.
Your gut wants to heal. It’s designed to heal. You just need to give it what it actually needs, not just a break from the things that hurt it.
If you’ve been fasting for your IBS and feeling good, that’s wonderful. But don’t stop there. Take the next step and address the root causes. Your future self will thank you.